Breadcrumbs
- Home
- Tools & Resources
- Key References
Key References

Order from Amazon.ca or contact us to purchase a copy!
“Once again, the educational team from the University of Toronto is providing cutting-edge work. With interprofessional education and care sweeping across the United States, academic programs will be looking for a resource such as this to provide guidance for building their educational models. The quality of this work is outstanding. The authors combine up-to-date IPE scholarship with practical content expertise that ill assist educators as they forge new IPE curricula and collaborative care learning opportunities for health profession students and clinicians alike.” — RICHARD D. KIOVSKY, INDIANA UNIVERSITY SCHOOL OF MEDICINE
Sioban Nelson is the Vice-Provost Academic Programs, University of Toronto. She is coeditor of Complexities of Care: Nursing Reconsidered and Notes on Nightingale: The Influence and Legacy of a Nursing Icon, both from Cornell, and the author of Say Little Do Much: Nursing, Nuns and Hospitals in the Nineteenth Century.
Maria Tassone is the inaugural director of the Centre for IPE. She is also the Senior Director, Interprofessional Education and Practice at the University Health Network in Toronto, and Assistant Professor in the Department of Physical Therapy, Faculty of Medicine, University of Toronto.
Brian D. Hodges is Vice-President Education at the University Health Network and Professor of Psychiatry, Scientist at the Wilson Centre for Research in Education, and Richard and Elizabeth Currie Chair in Health Professions Education Research at the University of Toronto. He is coeditor of The Question of Competence: Reconsidering Medical Education in the Twenty-first Century and author of The Objective Structured Clinical Examination: A Socio-History.
While informed by CACHE and TIER’s experiential knowledge from patient and student engagement work, voices in our healthcare and education systems, and research literature, we recognize that every context is different. We are working within a North American context from a team based in Toronto, Canada. We welcome insights from patients, students, educators, clinicians, faculty, staff, and leaders from other contexts (Farah.Friesen@uhn.ca).
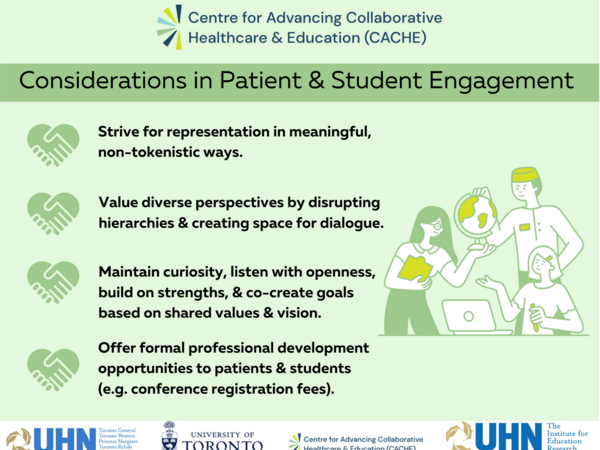
- Consider how to continually strive to engage patients and students from diverse backgrounds, “to represent the complex cultural, social, and economic complexions of contemporary society” (Rowland & Kumagai 2018). Scholarship in patient engagement has cautioned that usually individuals who are who are white, affluent, and older have time to take part in initiatives (Rowland & Kumagai 2018). In patient and student engagement, we must be aware so that the concerns and priorities of select demographic groups (often privileged) are not taken to reflect the needs of all.
- While striving for representation, consider how to include patients/clients/families/caregivers in meaningful, non-tokenistic ways. Guiding principles are a useful approach before patient or student engagement to ensure collaborative achievement of shared visions. In patient engagement, personal knowledge and lived experience are often invited; valuing this as expertise might also include considerations for patient recognition through remuneration.
- Ensure that diverse perspectives and experiences are invited and valued. This might necessitate brave/accountable spaces (Ahenkorah 2020) where power relations are explicitly addressed in order to disrupt hierarchies and share power (www.teachingfortransformation.com) - e.g. between patient/clinician or teacher/learner. Offering space where diverse views exist, without consensus, provides opportunities for dialogue, critical reflection (Kumagai & Naidu 2015; hooks 1994; Ng et al 2015; Ng et al 2019; Boyd et al 2022), and collaborative leadership.
- Maintain curiosity and listen with openness. Sometimes educators might assume that students are “not ready,” do not like uncertainty, and want “recipes” - yet we are striving to prepare learners for the realities of “indeterminate zones of practice - uncertain, unstable, unique, or value-conflicted practice situations” (Ng et al. 2015). Our work with student-led environments, Interprofessional Healthcare Students' Association (IPHSA), and the University of Toronto’s IPE Curriculum electives show that often students are craving new and different learning experiences while faculty might resist. Mentorship and support for students in combination with faculty development for educators ensures mutually beneficial, continual growth for all.
- Offer professional development opportunities to patients and students (e.g. support conference registration fees, invite to Community of Practice and other events). This recognizes patients and students as equally valued members of practice and education communities and integral collaborators in knowledge mobilization.
Select References on Patient & Student Engagement Considerations
- Ahenkorah E. Safe and Brave Spaces Don’t Work (and What You Can Do Instead). Medium. 2020. Full text
- Baker LR, Phelan S, Woods NN, Boyd VA, Rowland P, Ng SL. Re-envisioning paradigms of education: towards awareness, alignment, and pluralism. Advances in Health Sciences Education. 2021 Aug;26:1045-58. Full text.
- Brewer ML, Flavell HL, Trede F, Smith M. A scoping review to understand “leadership” in interprofessional education and practice. Journal of Interprofessional Care. 2016 Jul 3;30(4):408-15. Full text.
- Boyd VA, Woods NN, Kumagai AK, Kawamura AA, Orsino A, Ng SL. Examining the impact of dialogic learning on critically reflective practice. Academic Medicine. 2022 Nov 1;97(11S):S71-9. Full text.
- Chicago Beyond. Why am I always being researched? Research equity guidebook. https://chicagobeyond.org/researchequity/
- Health Quality Ontario. Engaging with Patients and Caregivers about Quality Improvement: A Guide for Health Care Providers. Full text.
- Jensen CB, Norbye B, Dahlgren MA, Iversen A. Patient participation in interprofessional learning and collaboration with undergraduate health professional students in clinical placements: A scoping review. Journal of Interprofessional Education & Practice. 2022 Jan 12:100494.
- Kumagai AK, Naidu T. Reflection, dialogue, and the possibilities of space. Academic Medicine. 2015 Mar 1;90(3):283-8. Full text.
- Kumagai AK, Naidu T. On time and tea bags: chronos, kairos, and teaching for humanistic practice. Academic Medicine. 2020 Apr 1;95(4):512-7. Full text.
- Lumague M, Morgan A, Mak D, Hanna M, Kwong J, Cameron C, Zener D, Sinclair L. Interprofessional education: the student perspective. Journal of interprofessional care. 2006 Jan 1;20(3):246-53. Full text.
- Ng SL, Forsey J, Boyd VA, Friesen F, Langlois S, Ladonna K, Mylopoulos M, Steenhof N. Combining adaptive expertise and (critically) reflective practice to support the development of knowledge, skill, and society. Advances in Health Sciences Education. 2022 Nov 9:1-7. Full text
- Ng SL, Kinsella EA, Friesen F, Hodges B. Reclaiming a theoretical orientation to reflection in medical education research: a critical narrative review. Medical education. 2015 May;49(5):461-75. Full text.
- Ng SL, Wright SR, Kuper A. The divergence and convergence of critical reflection and critical reflexivity: implications for health professions education. Academic Medicine. 2019 Aug 1;94(8):1122-8. Full text.
- Richards DP, Poirier S, Mohabir V, Proulx L, Robins S, Smith J. Reflections on Patient Engagement by Patient Partners: How It Can Go Wrong. Pre-print undergoing review full text.
- Rowland P, Anderson M, Kumagai AK, McMillan S, Sandhu VK, Langlois S. Patient involvement in health professionals’ education: A meta-narrative review. Advances in Health Sciences Education. 2019 Aug 1;24:595-617. Full text.
- Rowland P, Kumagai AK. Dilemmas of representation: patient engagement in health professions education. Academic Medicine. 2018 Jun 1;93(6):869-73. Full text.
-
Wong R, Kitto S, Kumagai AK, Whitehead CR. Paradox of patient-centered care and the implications for patient involvement in continuing professional development. Journal of Continuing Education in the Health Professions. 2021 Oct 1;41(4):238-46. Full text.
Key References for Collaboration Healthcare & Education
- Canadian Health Services Research Foundation, Teamwork in Healthcare: Promoting Effective Teamwork in Healthcare in Canada. June 2006.
- Canadian Interprofessional Health Collaborative (2012). An Inventory of Quantitative Tools Measuring Interprofessional Education and Collaborative Practice Outcomes.
- Canadian Interprofessional Health Collaborative (2024). National Competency Framework Quick Reference Guide.
- Carpenter, J. & Dickinson, H. (2008). Interprofessional Education and Training. Chapter 4 – measuring Outcomes using validated Measures. UK: The Policy Press.
- Cox et al., (2018). Measuring the impact of interprofessional education on collaborative practice and patient outcomes. Journal of Interprofessional Care, 30(1), 1-3.
- D’Amour, D. & Oandasan, I. (2005). Interprofessionality as the field of interprofessional practice and interprofessional education: An emerging concept. Journal of Interprofessional Care , 19 (Suppl 1): 8-20.
- Gordon, S., Mendenhall, P., & O’Connor, B. (2013). Beyond the Checklist: What Else Health Care can Learn from Aviation Teamwork and Safety. Cornell University Press, U.S.A.
- Hammick, M., Freeth, D., Koppel, I., Reeves, S. & Barr, H. (2007). A best evidence systemic review of interprofessional education: BEME Guide no. 9 Medical Teacher. 2007, Vol. 29, No. 8, pages 735-751.
- Implementing Interprofessional Care in Ontario. Ministry of Health and Long-Term Care. (2010).
- Interprofessional Care: A Blueprint for Action in Ontario. Ministry of Health and Long-Term Care. (2007).
- Nelson, S., Tassone, M. & Hodges, B. (2014). Creating the Health Care Team of the Future: The Toronto Model for Interprofessional Education and Practice. Cornell University Press, U.S.A.
- Reeves S., (2018) Ideas for the development of the interprofessional education and practice field: An update. Journal of Interprofessional Care 30(4), 405-407.
- Reeves S., Perrier L., Goldman J., Freeth D., Zwarenstein M. (2008). Interprofessional Education: effects on professional practice and health care outcomes. Cochrane Database of Systematic Reviews 2008, Issue 1.
- Romanow, R. (2002). Building on Values: The Future of Health Care in Canada. Final Report of the Commission of the Future of Health Care in Canada.
- Simmons, B., Oandasan, I., Soklaridis, S., Barker, K., Esdaile, M., Kwan, D., Leszcz, M., Lowe, M., Moaveni, A., Richardson, D., Silver, I., Sinclair, L., & Wagner, S. (2011) Evaluating the Effectiveness of an Interprofessional Education Faculty Development Course: The transfer of Interprofessional Learning to the Academic and Clinical Practice Setting. Journal of Interprofessional Care, 25(2):156-7.
- World Health Organization (WHO) Framework for action on interprofessional education and collaborative practice (2010)